Diverticulitis vs. Diverticulosis Nutrition
Digestive health (like managing diverticulitis vs. diverticulosis) is vital for well-being and nobody knows this more than our guest blogger, dietitian extraordinaire, Andrea Hardy from Ignite Nutrition Inc. Andrea is an influential, Calgary-based dietitian and TED-X speaker with a contagious (and unifying) “science-first” mentality. Andrea’s team is Calgary-based but offer virtual visits as well. She and I have been friends for years, and I’m thrilled to have her share nutrition tips and break down the science for us today.
Today, Andrea will be addressing a timely topic, Nutrition for diverticulitis vs. diverticulosis: What You Need to Know.

What’s the Bowel?
The human bowel is a complex place in which there are many important structural elements, including sphincters, valves, smooth muscles and mucosa (to name a few). Moral of the story – the digestive tract isn’t a basic food tube. There are lumps, bumps, and divots that are completely normal. However, there are also structural abnormalities that can be problematic in the bowel and prevent digestive processes from working properly.

One of these potential structural issues is called diverticula, which are herniations (or pockets) that can form within the walls of the intestines. These pouches can be small or large, but are often only as small as 5 to 10 millimetres in diameter. Diverticula mostly develop in the sigmoid colon (the last part of the large intestine) but can develop throughout any part of the small or large intestines. For many, having diverticula is a big health concern. As the diverticula can become inflamed and infected, it can result in gastrointestinal symptoms and poor quality of life.
Diverticulitis vs. Diverticulosis
Curious about diverticulitis vs. diverticulosis? Diverticular disease is an umbrella term we use to encompass two different disease states – diverticulosis and diverticulitis. Although these words look pretty similar, they are indeed quite different. Let’s break it down:
Simply defined, diverticulosis is the presence of diverticula (those tiny pouches in the intestines) and is actually very common, especially with ageing. Many people have diverticulosis without any significant symptoms or complications.
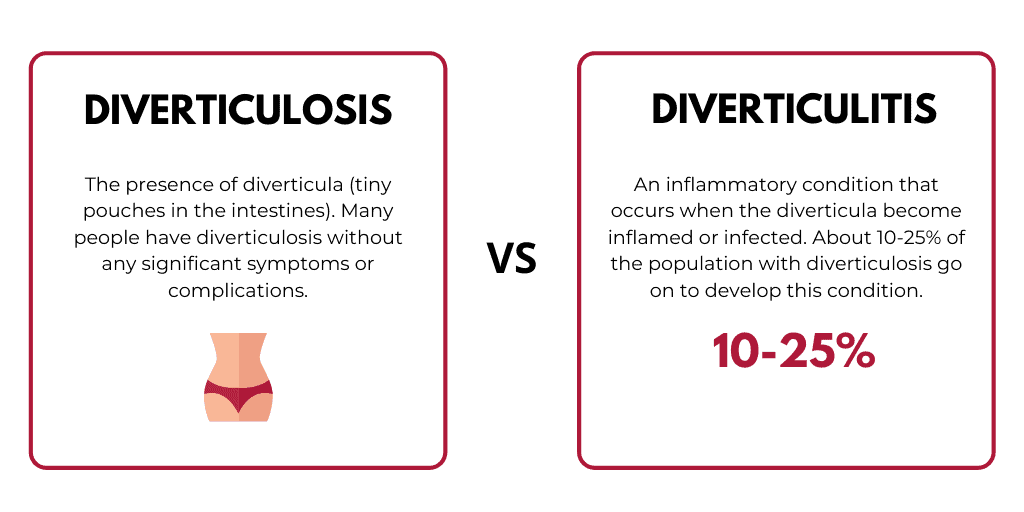
Conversely, Diverticulitis occurs when the diverticula become inflamed or infected. About 10-25% of the population with diverticulosis go on to develop this inflammatory condition. We’ll be reviewing this today and how nutrition and lifestyle can reduce symptoms and long-term risks associated with diverticulitis.
Symptoms of Diverticulitis
As mentioned above, many people go years (or even a lifetime) without showing any symptoms of diverticular disease. Many people don’t even know they have it!
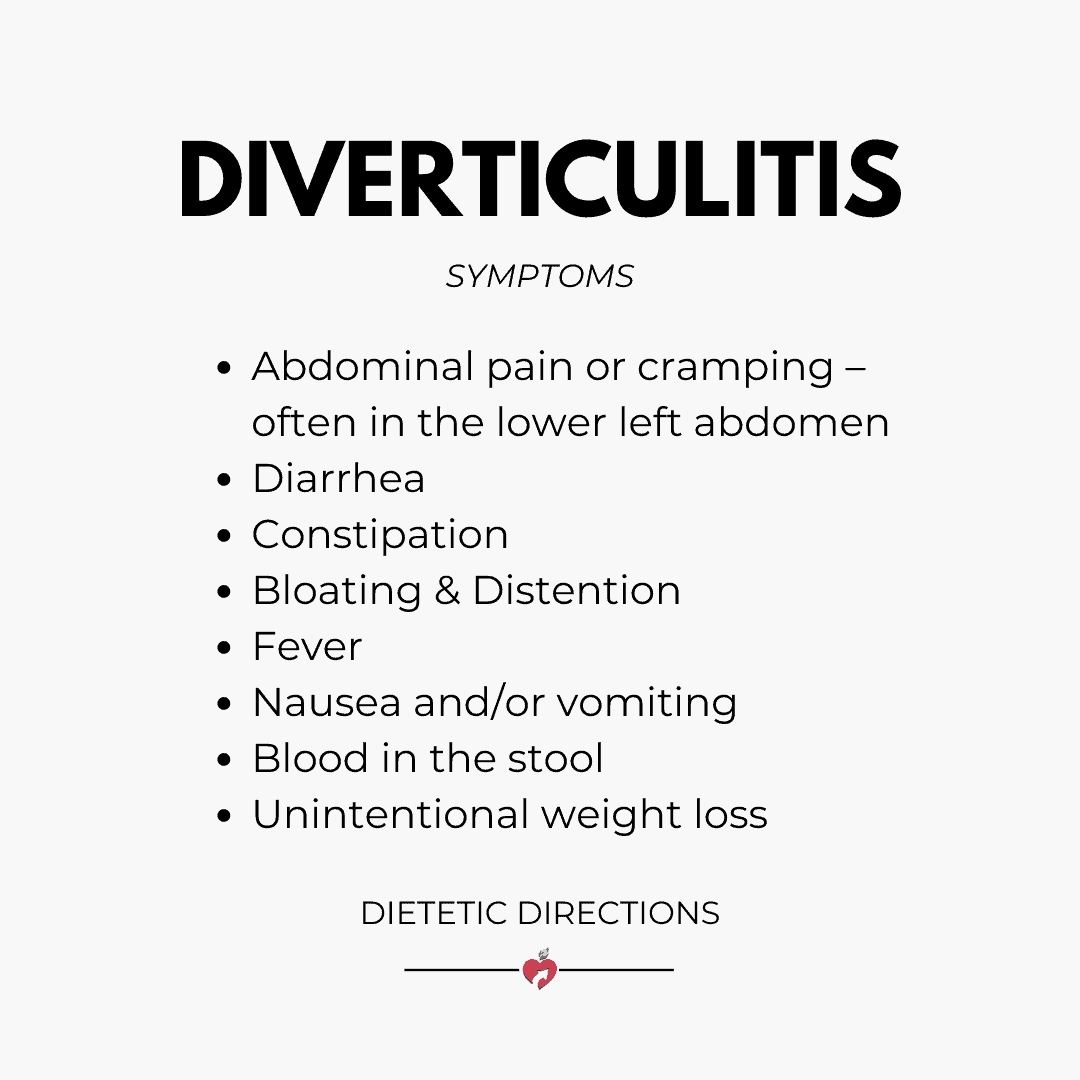
However, when the pouches become infected and/or inflamed, the following symptoms can occur:
- Abdominal pain or cramping – often in the lower left abdomen
- Diarrhea
- Constipation
- Bloating & Distention
- Fever
- Nausea and/or vomiting
- Blood in the stool
- Unintentional weight loss
With reoccurring diverticulitis flare-ups, individuals are at higher risk of bowel obstruction, fistula, or abscess (pus collecting in the diverticula).
Flare-ups of diverticulitis can be very short-term or extended over a longer period of time.
Diagnosing Diverticulitis
Like many digestive disorders, the symptoms of diverticulitis are non-specific and can be linked to a number of different conditions including irritable bowel syndrome, Crohn’s or celiac disease.
Although the symptoms are very similar to IBS, the diagnosis of diverticulitis differs because diverticula are structural and can be detected on imaging. IBS, on the other hand, is diagnosed symptomatically – it won’t have anything “show-up” in imaging. Diagnosis of diverticulosis (the non-inflamed state) often occurs during a routine colonoscopy, such as the one many people get around age 50.
In contrast, diagnosing diverticulitis is most often after a sudden, painful attack causing symptoms such as the ones listed above. Due to the nonspecific nature of these symptoms, diverticulitis can be difficult to pinpoint right away, especially if someone is not aware they have diverticula in their bowel.
In order to diagnose diverticulitis, your healthcare team may do any or all of the following:
- Comprehensive assessment – looking at your past medical history, family medical history, symptoms, and lifestyle
- Physical exam
- Collection of blood samples to assess complete blood count and detect inflammation in the body
- Urinalysis
- Abdominal imaging, including x-ray, CT, or ultrasound
- Referral to a gastroenterologist for a colonoscopy
Management of Diverticulitis
Treatment of diverticulitis can differ based on the severity of abdominal pain, fever, and other symptoms and combines both dietary and antibiotic treatment. In extreme cases, people may also require hospitalization or surgery in order to adequately recover from an infection of the diverticula.
Diverticulitis Nutrition
The initial dietary management of a sudden diverticulitis flare-up often consists of a short-term clear fluid diet, meaning the patient consumes only liquids such as water, juice, jello, and broth. This allows antibiotics to start working and allows the gut to rest. As well, this helps to clear out material that may be caught in their diverticula pouches, which can cause bowel obstruction and pain. Being full of stool or constipated is often linked to poor diverticulitis outcomes, so the goal of the clear fluid diet is to reduce the amount of fibre (and therefore fecal matter) in the colon.
Fibre Confusion
From there, as inflammation and symptoms reduce, more solids and fibre can be added back into the diet gradually. The goal is to work toward a low fibre diet of about 10-15 grams fibre daily for a short period of time. Due to the specific requirements of this diet, it is best to work with a dietitian. They can help to identify the fibre content of different foods, ensure you get enough overall nutrition, and prevent unintentional weight loss.

Within a few weeks of an acute diverticulitis attack, most people can work toward a higher fibre diet as their symptoms continue to subside. For women, this is around 25 grams of fibre daily and for men, 38 grams.
FODMAP Diet for Diverticulitis?
Another emerging area of dietary research is on the low FODMAP diet for diverticulitis. Although the low FODMAP diet was developed for irritable bowel syndrome, there are some studies to suggest it could be beneficial for those with diverticulitis as well. The theory behind this is that increased pressure in the colon can irritate diverticula. Lots of pressure and gas in the bowel is likely to push on the mucosa of the colon, creating pouches or enlarging the pouches that already exist. Therefore, a diet lower in FODMAPs may improve symptoms. However, this is still a relatively new area of research for diverticulosis and consideration of a low FODMAP diet (or any elimination diet) should be discussed with a registered dietitian first.
No Nuts and Seeds?
In the past, many believed that small particles of food such as seeds, nuts and popcorn would worsen diverticulitis or increase the incidence of diverticulitis attacks. The literature has since unfounded this and consider these foods safe to consume – particularly during remission of diverticulitis. In fact, they are quite healthy for us! Nuts and seeds offer lots of healthy fats that actually help to reduce inflammation in the body.

That being said, it may still be beneficial to reduce our intake of these foods during diverticulitis flare-ups, as they are higher in fibre than other foods.
Bottom Line
We hope we’ve cleared up the confusion on diverticulitis vs. diverticulosis. Remember that having diverticula is common, particularly in the aging population and is often completely asymptomatic. Diverticulitis treatment in most cases requires dietary changes, specifically a reduction in dietary fibre to allow the gut to rest and clear fecal matter from the colon. Working with a dietitian is highly recommended to help take care of diverticulitis vs. diverticulosis and those uncomfortable symptoms that may occur.




